Experts are raising alarms following recent statements:
Minimized risks of the birth control pill? Here are 3 dangers that nearly every woman overlooks.

And yet, taking the pill every day feels like the norm because "everyone" does it?
For a long time, that was my reality. The pill was as routine as brushing my teeth.
Then one evening, I found myself staring at the blister pack, questioning:
"What exactly am I swallowing – and why is there so little discussion about the obvious side effects?"
So, I started researching. First, I browsed self-help sites, then official materials for doctors, and eventually, extensive clinical studies.
I quickly realized: This isn't just internet gossip – it's about official and academic warnings that highlight rare but serious risks associated with birth control pills.
The deeper I delved, the clearer a pattern emerged. Beyond the common "minor" side effects, three recurring issues appeared in professional texts, guides, and clinical studies.
Three dangers that many of us may never encounter, yet every woman should be aware of before making a decision.
I promise you: This article won't incite panic or deliver a moral lecture.
It's an informative overview – detailing what official sources say about birth control pills, what researchers report, and how this impacts your daily life.
Only after that will we explore hormone-free contraceptive alternatives – from apps and temperature methods to direct hormonal signals from your own body.
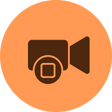
Danger #1 - The little asterisk in the leaflet: What many people often realize too late about blood clots.
blood clots can occur rarely, but they are serious when they do.
What exactly is a "blood clot"?
A clot is a blockage that can obstruct a blood vessel. It often starts in the leg (swelling, warmth, pain in the calf). If the clot dislodges and travels to the lungs, it can lead to a pulmonary embolism (sudden shortness of breath, chest pain, rapid heartbeat).
Why is this highlighted in official information?
Because authorities and expert committees have been emphasizing for years: the risk is rare but real. Doctors receive a checklist for initial prescriptions, and users get a patient card with warning signs.
In short: this is not just an internet myth, but an official standard for awareness.
Who should be particularly vigilant?
Even without technical terms, the rule of thumb is clear: the more additional factors, the closer you need to look. These include smoking, prolonged sitting/air travel, family clotting issues, severe migraines with aura, or recent childbirth.
Especially in the first months after starting a new pill, the risk is highest—hence, recognizing warning signs is crucial.
I realized: this is not an internet rumor, but officially documented. If a medication requires a patient card and a checklist, then this topic must be included in every fundamental decision about contraception—especially for first-time users.
As soon as I saw these documents, another question arose: "What about the numerous reports of negative effects of the birth control pill on mood and mental health?"
Danger #2 – When moods shift: Data-driven indications of depressive symptoms.

The question is: are there solid indicators that this is related to the birth control pill?
In short: yes, there are clear connections that should be acknowledged.
The largest data point:
A Danish registry study involving over 1 million women examined what happens after starting hormonal contraception. The result: users were more likely to be treated for depression for the first time or received a depression diagnosis—most notably among teenagers.
Important: this indicates a correlation, not "proof that the pill causes depression." However, it serves as a significant warning signal that should be taken seriously.
And what do official guides say?
The British NHS explicitly lists mood swings and depressive moods as possible side effects of the birth control pill—alongside rare but serious risks like blood clots. This means that even neutral public health organizations acknowledge that mood can be an issue.
This chapter struck a chord. Mood is not a "soft topic." When millions of data points signal a trend and even official bodies mention it, it must be included in educational texts.
However, a third area is almost always brought up in discussions—not life-threatening, but very relevant:
Danger #3 – Decreased Desire, Less Intimacy: How the Pill Can Lower Sexual Function and Libido

The NHS also lists reduced libido among the common side effects, alongside increased blood pressure, headaches, and breakthrough bleeding. For those affected, this is not a minor detail but a reality in their relationships.
For me, that was the final straw. Official warning materials about blood clots, extensive databases on depressive moods – and real-life consequences for relationships affecting a large number of users.
What conclusion did I draw from this?
Exploring hormone-free alternatives.
I started researching in health forums, on social media, and in studies to find out what popular contraceptive options exist for women that won’t disrupt hormonal balance.
I quickly discovered two innovative methods – here’s a brief overview:
Alternative 1 – Period Calendar Apps: Attractive Predictions, Little Certainty

From this historical data, it calculates my likely fertile days and colors my month in cheerful hues. For everyday tracking and a sense of order, it’s quite pleasant—I can see at a glance when my next period is due and jot down notes about my mood, sleep, or exercise.
However, when it comes to contraception, comfort turns into a false sense of security.
Real cycles are inherently dynamic!
Stress, travel, illness, or short nights can shift patterns that the app can only access retrospectively. The nicely marked windows are ultimately just vague predictions, not 100% guarantees.
I’ve caught myself trusting the pretty interface more than it deserves: the app calculated, while my body did its own thing.
My conclusion: great for awareness and documentation—far too vague as a basis for contraception…
Alternative 2 – Temperature Apps and Devices (BBT)

A thermometer (or sensor) provides a value every morning, and apps chart the curve, marking "safe" and "unsafe" days.
This sounds a bit more like data control—until you grasp the crucial point: temperature rises after ovulation, triggered by progesterone.
For contraception, this presents a timing issue because the fertile window occurs before the reliable rise. Practically, BBT requires strict routine, consistent measurement times, and adequate sleep.
Factors like alcohol, illness, shift work, or a stressful morning can distort the picture. After a few restless nights, I saw how quickly a clean curve can wobble, and the algorithm ends up guessing more than knowing.
This technique reduces effort but doesn’t solve the fundamental problem:
The predictions are inaccurate, and you only get reliable information in hindsight…
After considering these two alternatives, it became clear to me: calendar apps and temperature methods remain rough estimates. Temperature reveals information only afterward; calendar apps guess based on past data. I craved real certainty…
One question lingered in my mind:
If the hormone progesterone triggers the temperature rise—why not just measure progesterone directly?
Before we dive into that, here’s a quick overview of progesterone:
Progesterone: A Key Hormone in the Cycle
After ovulation, the body releases progesterone—it prepares the uterus for a potential pregnancy and simultaneously causes the basal temperature to rise.
If fertilization doesn’t occur, the progesterone level drops at the end of the cycle, and menstruation begins.
For cycle tracking, progesterone is an ideal marker: it indicates whether and when ovulation has occurred.
Theoretically, daily progesterone measurement would be the gold standard for accurately determining fertile and infertile phases. However, in practice, this has been challenging—progesterone is typically tested in the blood, requiring regular lab tests.
The innovation that now makes this possible from home comes from a Berlin-based Femtech startup that has found an easier way:
Measuring progesterone through saliva, conveniently from home. Saliva contains small amounts of the hormone, and with a sensitive testing method, this level can be determined daily.
This is now possible—a mini-laboratory for home use makes it feasible to check progesterone levels every day.
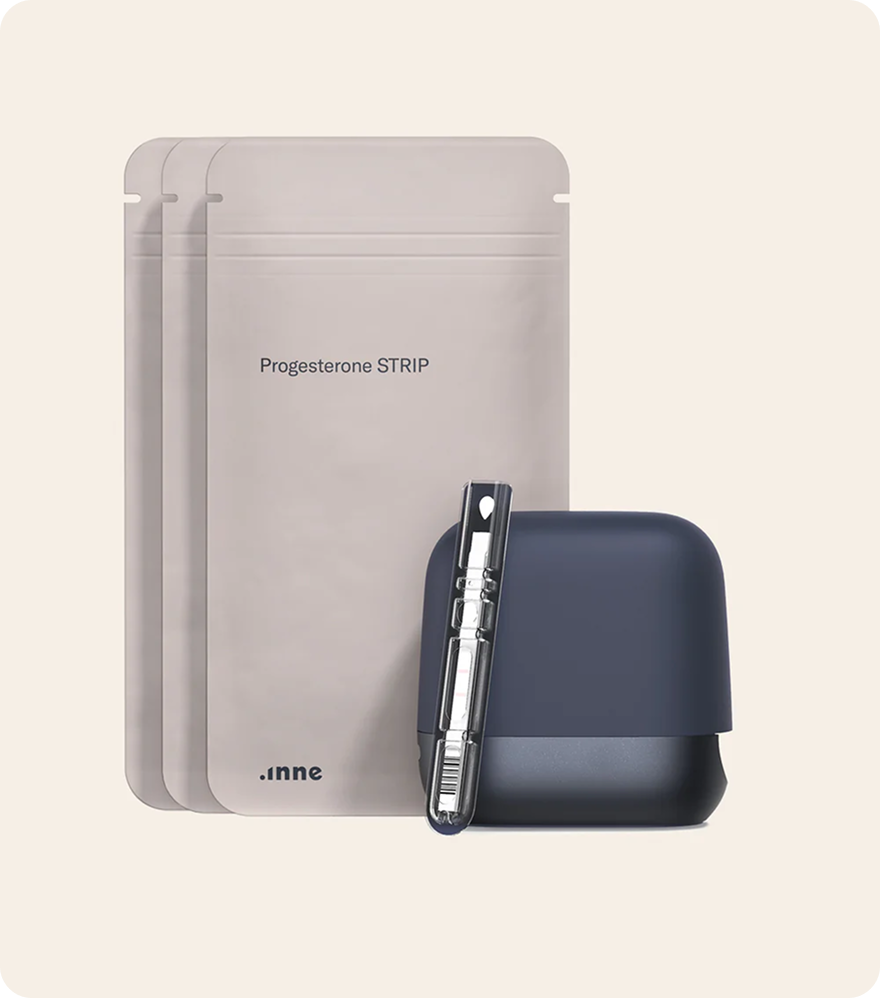
High-Tech in the Bathroom: Saliva Test Replaces Thermometer

The technology resembles that of COVID-19 rapid tests or pregnancy tests: A lateral flow immunoassay uses antibodies on a test strip that produce a color change when they come into contact with progesterone.
The application is straightforward: During the daily window from 5 AM to 2 PM, the user places a drop of saliva on a special test strip and inserts it into a small reader. This device scans the strip and measures the progesterone level in the saliva.
The results are transmitted via Bluetooth to an app on the smartphone, which processes and displays the hormone curve. A significant rise in progesterone indicates that ovulation has recently occurred.
In the initial cycles, the system learns the individual values of the user. After two to three months, an algorithm can even predict when the next ovulation is expected.
This not only confirms past events but also provides increasingly accurate predictions of fertile days. Founder Rapti envisions that every woman should gain insight into her own body to make informed decisions about sexuality and health.
Supported by an international team of experts, her startup has brought the idea of the progesterone saliva test to market in just a few years.
I was eager to test the progesterone measurement method myself.
Cycle Tracker in Practice: What This New Mini-Lab Can Do

The kit includes the handy inne Reader, disposable test strips, and the inne app for smartphones. The application integrates surprisingly easily into the morning routine.
Each day, a test strip is moistened with saliva and inserted into the reader—after about 15 minutes, the result appears in the app.
One user reported in her review that the saliva sample in the morning became a "completely natural" part of her daily routine within just a few days. Unlike the tedious temperature measurement, there’s no need to measure at the exact same minute; instead, there’s a comfortable window between 5 AM and 2 PM.
No need for a wake-up call in a sleepy state—the app sends a notification if you might forget to take the test. In just a few seconds, the saliva sample is taken, completing the measurement. Afterward, you can relax and continue with your daily routine while waiting for the result—the progesterone level for the day is saved in the app.
Testers found the view of their personal hormone curve in the app particularly fascinating. For the first time, they could see in black and white (or color-coded in the app) what was happening hormonally in their bodies. "When my progesterone level visibly rose after ovulation—that was such a wow moment," described one user.
"I knew: Okay, my ovulation really happened. I never had that clarity with other methods." This 'aha' moment—the certainty that the body is functioning and knowing when the infertile phase begins—gives many users a sense of confidence and trust in natural contraception.
The mini-lab also impresses in terms of design and usability. The dark blue reader device looks high-quality and discreet—"not a clunky piece of tech, but something you’d happily place on your nightstand," as one tester noted.
The connection to the smartphone works smoothly, and the app is intuitive and easy to navigate. Users can also make manual notes—tracking mood, cervical mucus observations, and symptoms—complementing traditional NFP methods.
Effectiveness and Conclusion: Can the Saliva Test Replace the Pill?
A recent study in Berlin involving 300 women provides promising data: The supervising experts rated the contraceptive method with a 100% safety rating under perfect professional application.
In other words, the concept works—but it depends on the user’s reliability, similar to condoms or the pill (where errors in usage can also lower effectiveness).
The Pearl Index of the inne system is expected to be on par with other modern methods. The startup claims an effectiveness of 92% with perfect use, comparable to typical pill usage.
Who is this method particularly interesting for? Mainly women who wish to avoid hormones for health or personal reasons but still value a high level of safety and knowledge about their own bodies.
For them, the inne Minilab offers a unique alternative. Instead of blindly trusting that "somehow they won’t get pregnant," daily hormone readings provide concrete feedback.
Women trying to conceive also benefit: they not only see when their fertile days are but also receive confirmation that ovulation has indeed occurred—crucial information when pregnancy doesn’t happen right away.
Even those who have just stopped taking the pill and want to better understand their natural cycle can gain valuable insights from the data.
Of course, such a device doesn’t replace a visit to the doctor in all situations. However, for a growing number of health-conscious women, it means regaining a degree of self-determination without sacrificing responsible contraception.
The days when hormone-free contraception equated to uncertainty seem to be over. The "pill" has gained competition—high-tech and hormones are no longer mutually exclusive. Whether the saliva test will revolutionize contraception remains to be seen. But it’s already clear: it expands options and sheds new light on the female cycle—precise, personal, and hormone-free.

 4.8/5
4.8/5
 4.4/5
4.4/5
Over 15K+ women trust inne
Can I use inne?
inne is currently a good fit for women who for the last three months can relate to these criteria
I am not pregnant
During pregnancy, you do not have a menstrual cycle. Therefore you should wait until the second consecutive period after the end of the pregnancy, even if the pregnancy was not carried to term before starting to use inne.
I am not breastfeeding
When breastfeeding, your hormone levels might fluctuate and your menstrual cycle is not regular. Therefore you should wait until the second consecutive period after you stopped breastfeeding before starting to use inne.
I am not on a treatment that affects my cycle
Medical treatments that can affect your cycle, should indicate so in the patient information leaflet of the respective medication. The inne minilab measures how your progesterone behaves during the menstrual cycle. If our menstrual cycle is affected due to another treatment we won’t be able to provide you with accurate evaluations.
I do not have polycystic ovarian syndrome
If you suffer from PCOS, your hormonal cycle might not be regular and this might affect the accuracy of your system. We hope we will be able to support women who have polycystic ovarian syndrome in the future.
I do not have endometriosis
If you suffer from endometriosis, your hormonal cycle might not be regular and this might affect the accuracy of your results. We hope we will be able to support women who have endometriosis in the future.
I am not experiencing menopausal symptoms
Menopausal symptoms can be hot flashes and night sweats. During menopause, your hormone production decreases and can fluctuate. We hope we will be able to support women during menopause in the future.
My cycle is between 22 and 35 days long
For now, we can ensure the accuracy of the results for cycles between 22 to 35 days long. We are always working on making our system available for a wider variety of cycles. Please note that inne can only provide accurate results when you add correct dates during the inne APP onboarding.
I am older than 18 years old
The inne minilab is a medically certified system for fertility monitoring. It is intended for women above 18 years old.
I am not on hormonal contraception
Hormonal contraception affects your natural hormone levels. You should have had two consecutive cycles after you stopped using hormonal contraception before you start using inne.